Benoy Mathew: Understanding FAI Syndrome
Een gastblog van docent Benoy Mathew.

Historically, most hip osteoarthritis (OA) was generally thought to be ‘wear and tear’ or idiopathic in origin. For the last 15 years, there has been suggestion that development of idiopathic hip OA could be, partly, explained by structural abnormalities in femur and acetabulum. One of the common morphological variations, Femoro – Acetabular Impingement (FAI) has been increasingly recognised as a source of hip and groin pain in the active population. Over time, it has been hypothesised that these morphological variations can put stress on hip joint and could lead to degenerative changes in certain high-risk individuals.
The prevalence of radiological FAI is a common finding in asymptomatic active individuals (1). Three types of morphological variations have been described in FAI: Cam, Pincer and mixed. Fortunately, very few develop clinical symptoms and current evidence does not support prophalytic screening for FAI in the asymptomatic population (2). A radiological finding of FAI is not sufficient for the diagnosis of FAI, since it is a clinical diagnosis, based on clinical history, physical examination and relevant imaging.
So, how do you define symptomatic FAI?
A recent consensus meeting defined FAI as “ a clinical entity in which a pathological mechanical process causes hip pain when morphological abnormalities of the acetabulum and/or femur, combined with vigorous hip motion (especially at the extremes), lead to repetitive collisions that damage the soft-tissue structures within the joint itself. ” (3).
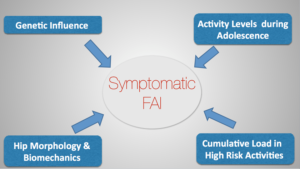
Let us examine some contributing factors which have been linked with the aetiology of FAI in the active population.
Genetic Factors
It has been reported that the relative risk of having a cam or pincer deformity in siblings of patients with cam or pincher type FAI is nearly three times (4). Another study had shown that the morphological evidence of FAI was more common in white women as compared to Chinese women (5). Further, the prevalence of cam deformity is higher in men compared with women (6). These studies suggest there could be a genetic influence, leading to the development of FAI.
Developmental Factors
It has been shown that cam-type deformity develops around the age of 10-12 years (7) and does not progress after the closure of the growth plate in the athletic population (8). Therefore, one can assume that cam type deformity is related to skeletal development. Further, there is a link between training intensity and frequency with the radiological signs of FAI. Athletes with excessive participation in high-impact athletic activities such as football, ice hockey and basketball during adolescence when the skeleton is maturing have a higher incidence of FAI (9-11). It is believed that the high shear forces at the antero-superior head-neck junction of the growing hip leads to changes in the shape of the growth plate.
Morphological Variations
Individuals with restricted hip internal rotation have a higher risk of developing hip pain (12). The combination of a cam deformity along with restricted hip internal rotation can increase the likelihood of symptomatic FAI in the athletic population (13). Decreased range of motion, especially hip internal rotation may subject the hip stabilisers to greater stress, leading to soft tissue damage (14). Other morphological factors such as femoral anteversion, torsion and neck-shaft angles and variation in acetabular anatomy can also contribute to the appearance of clinically symptomatic impingement (15).

Cumulative Overload
FAI is a motion-dependent process and is linked with the musculo-skeletal loading on the hip joint, which is directly related to the physical activities undertaken by the athlete. People who are involved in sports which involve vigorous hip motion (especially end-range flexion and internal rotation) are more likely to develop clinical FAI, in the presence of cam or pincer type morphology (16). Athletes who trained four or more times per week had higher incidence of cam-type FAI than those who trained three or less times (11). Sports such as football and ice-hockey that involve extreme ranges of hip motion and high impact movements have a higher incidence of FAI (17).
Figure 1- Multi-factorial Aetiology of Symptomatic FAI
Conclusion
The mechanism leading to the clinical syndrome of FAI in certain individuals is not currently well understood. As a clinician, it is important to understand the multi-factorial nature of FAI (Figure 1), while evaluating an active patient with chronic hip related groin pain. At this point of time, there are no high-quality trials on conservative management of FAI. Based on current evidence, it is hypothesised that radiological changes of FAI develop during adolescence due to repetitive and intense loading, especially during extreme range of motion (17). However, the current evidence is not decisive and further high quality studies are needed to understand this complex condition.
I hope you found this short blog useful in understanding FAI and thanks for reading,
Ben

Ben works as an MSK Extended Scope Practitioner in the NHS and also in private practice. He has developed special interest in treating overuse lower limb pathologies, running injuries and chronic hip and groin patients. He is passionate about application of research in clinical practice and is involved in regular teaching nationwide on multiple lower limb courses.
Twitter @function2fitnes
Curious for more?
Come join us for Benoy Mathews course ‘The Adult Hip Patient’ in September!
References
- Laborie L, Lehmann T, Engesæter I, et al. (2011). Prevalence of radiographic findings thought to be associated with femoro-acetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology, 260(2), 494–502.
- Anderson et al. (2015). Radiographic Abnormalities Common in Senior Athletes With Well-functioning Hips but Not Associated With Osteoarthritis. Clin Orthop Relat Res, DOI 10.1007/s11999-015-4379-6.
- Sankar WN, Nevitt M, Parvizi J, et al. (2013). Femoro-acetabular impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthop Surg, 21 (Suppl 1): S7–15.
- Pollard TC, Villar RN, Norton MR, Fern ED, Williams MR, Murray DW, et al. (2010). Genetic influences in the aetiology of femoro-acetabular impingement: a sibling study. J Bone Joint Surg Br, 92, 209–16.
- Dudda M, Kim YJ, Zhang Y, Nevitt MC, Xu L, Niu J, et al. (2011). Morphologic differences between the hips of Chinese women and white women: could they account for the ethnic difference in the prevalence of hip osteoarthritis? Arthritis Rheum, 63, 2992–9.
- Gerhardt MB, Romero AA, Silvers HJ, et al. (2012). The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med, 40(3), 584–8.
- Agricola R, Bessems JH, Ginai AZ, et al.(2012). The development of cam-type deformity in adolescent and young male soccer players. Am J Sports Med, 40(5), 1099–106.
- Agricola R, Bessems JH, Ginai AZ, et al. (2014). A cam deformity is exclusively and gradually acquired during skeletal maturation: a prospective study with a minimum of 2 years follow-up. Am J Sports Med, 42(4), 798–806.
- Mariconda M, Cozzolino A, Di Pietto F, et al. (2014). Radiographic findings of femoroacetabular impingement in capoeira players. Knee Surg Sports Traumatol Arthrosc, 22(4), 874–81.
- Philippon MJ, Ho CP, Briggs KK, et al. (2013). Prevalence of increased alpha angles as a measure of cam-type femoroacetabular impingement in youth ice hockey players. Am J Sports Med, 41(6), 1357–62.
- Tak I, Weir A, Langhout R, et al. (2015). The relationship between the frequency of football practice during skeletal growth and the presence of a cam deformity in adult elite football players. Br J Sports Med, 49(9), 630–4.
- Ecker TM, Tannast M, Puls M, Siebenrock KA, Murphy SB. (2007). Patho-morphologic alterations predict presence or absence of hip osteoarthrosis. Clin Orthop Relat Res, 465, 46-52.
- Khanna et al. (2014). Incidence of Hip Pain in a Prospective Cohort of Asymptomatic Volunteers. Is the cam deformity a risk factor for hip pain? The American Journal of Sports Medicine, 42(4), 793-797.
- Voos et al (2010). Femoroacetabular Impingement in the Athlete: Compensatory Injury Patterns, Operative Techniques in Orthopaedics, 20(4), 231- 236
- Audenaert EA, Peeters I, Vigneron L, Baelde N, Pattyn C (2012). Hip Morphology characteristics and range of internal rotation in femoral impingement. Am J Sports Med, 40(6), 1329-1336.
- Agricola, R. (2014). Is osteoarthritis the price to be paid for a professional football career? or can we prevent it? Aspetar Sports Medicine Journal, 266 – 271
- Zadpoor, A. (2015). Etiology of femoro-acetabular impingement in athletes: A review of recent findings. Sports Med, Published Online: 22 May 2015.